
Artificial and augmented intelligence are driving the future of medical imaging. Tectonic is the only way to describe the trend. And medical imaging is at the right place at the right time. Imaging stands to get better, stronger, faster and more efficient thanks to artificial intelligence, including machine learning, deep learning, convolutional
neural networks and natural language processing. So why is medical imaging ripe for AI? Check out the opportunities and hear what experts have to say—and see what you should be doing now if you haven’t already started.
Let’s put the ridiculous aside. Radiologists will be empowered by AI, not replaced by it. Radiology has bought into the now-famous quote from Curtis Langlotz, MD, PhD, professor of radiology and biomedical informatics and director of the Center for Artificial Intelligence in Medicine and Imaging (AIMI Center) at Stanford University: “Artificial intelligence will not replace radiologists … but radiologists who use AI will replace radiologists who don’t.” It’s the rallying cry.
Medical imaging’s present and future is human plus machine. Radiologists are intrigued with AI’s potential to expedite and improve their ability to interpret images. Some are starting to benefit from AI apps, and test plenty more of their own and commercial apps in development. Like many other industries, healthcare looks to AI to quickly wring insights from data, making information more useful and actionable. Machines can’t think, but they can learn. Radiology is learning how they will mold the future.
Now is the time to get onboard and embrace AI, says the president of radiology’s leading professional association. “AI has the potential to enhance our profession and transform the practice of radiology worldwide,” RSNA President Vijay Rao, MD, told those gathered in Chicago for the profession’s largest stage at the 2018 annual meeting. “It will allow radiologists to spend more time on initiatives that will benefit both patients and physicians.”
Job one is recreating and rebranding reading rooms into digital diagnostic data hubs delivering “total imaging care,” says Rao, who is the chair of the department of radiology at Jefferson University Hospitals in Philadelphia. Radiologists must be present with patients, referrers and care decision-making.
“If you generate more useful data, you become a better consultant,” agrees Gary Wendt, MD, MBA, enterprise director of medical imaging and vice chair of informatics at the University of Wisconsin School of Medicine and Public Health in Madison. “If you’re actually giving more people more actionable data, you as a physician are a more valuable part of the care process.”
Rao sees the digital diagnostic data hub as a gathering place for clinical teams to meet or participate virtually through video conferencing to make decisions regarding patient care. Radiologists could someday rely on AI to aggregate current imaging findings with priors from other clinical departments and social determinants of health. Lab results, surgical or biopsy findings, health history, physical exams, patient demographics, patient genomics and risk factors also can be gathered and integrated into the overall clinical analysis.
“What’s hiding in this data that we’re not acting on, that we need to be doing right now to help our patients?” asks Brandon Fornwalt, MD, PhD, a radiologist and data scientist who serves as co-director of the Cardiac Imaging Technology Lab (CITL) within Geisinger’s Department of Imaging Science and Innovation. Researchers and radiologists are on a mission to find out.
Richard Bruce, MD, a neuroradiologist and medical director of radiology informatics at Univeristy of Wisconsin School of Medicine and Public Health, offers another perspective. He says AI is not necessarily always about providing something completely new “but about how to simply bring attention to the things that are already there. How do we reduce the noise? How do we bring to the top all those related things … so we can paint the most compelling picture, story, of the patient.”
Rao calls her vision the “total imaging care delivery model.” Instead of the referring physician leading the charge for patient communication, the radiologist can take over all aspects of imaging care for patients, which includes communicating results to the patient. “AI and related technologies give us the exact tools we need to finally make this vision a reality,” she says.
Just What The Doctor Ordered
At the dawn of AI in the 1950s, researchers sought to produce an intelligent system capable of passing the Turing test: Can a machine’s intelligence be made indistinguishable from that of a human? We are getting there. The last 70 years have seen alternating cycles of hope and despair, but a decade ago that began to change. The trajectory has been steadily moving up since as AI began to learn without having to be programmed. Today, both consumable data and computing power have increased by orders of magnitude, with more widespread affordability.
In AI, medical imaging sees opportunity amongst obstacles to improve access and quality, reduce cost, make the patient experience better—and don’t forget the caregivers. Meanwhile, more than 4 billion people lack access to medical imaging expertise, according to estimates from the World Health Organization. AI could offer solutions to clinician shortages across the globe and lack of access in some areas by offering remote reading options.
Obstacles lie along the imaging chain in image acquisition, reconstruction, exam positioning and quality control. AI has the potential to rid radiologists of repetitive lower-value tasks to bring time savings and accuracy boosts. It can identify disease with greater accuracy, reduce treatment variability and improve care processes and patient outcomes. It can detect hard-to-see lesions and decrease false-negative interpretations.
AI tools also can enhance image reconstruction, utilizing data more effectively and improving distorted or damaged images. Better worklist prioritization allows the sickest patients to receive quicker diagnoses and treatment, even in hospital settings in which radiologists are not immediately available. And radiology reporting gains consistency.
Machine intelligence is also helping to explore and expose key EHR data to provide a holistic view of the patient. More intuitive interfaces are being created based on caregiver types and easing documentation fatigue.
Beyond individual AI apps, the differentiator for both imaging and healthcare is going to be looking at large, longitudinal datasets, offers Geisinger’s Fornwalt. “Where you take a little cross-section of data and look forward and predict from that. That’s what machines are good at. We can’t do that as physicians…So we’re going to leverage that predictive power to make a difference.”
The advantage AI brings is a deeper look into the data, Bruce agrees, and “a recognition that there are opportunities to do more with what we’re acquiring and what can we unlock.” Machine intelligence sees more, differently, which “simply is just not possible no matter how much time a human sits looking at it.”
And truth be told, humans are often sitting too long these days.
Burnout is a big issue in radiology, with some 45 percent of radiologists reporting they are burned out, according to recent stats from Medscape that show consistency with last year. “We’re talking about data-driven, evidence-driven tools, and we need that,” Radiologist Paul Chang, MD, medical director of enterprise imaging at the University of Chicago, said in a presentation at RSNA 2018. “We need the help, because many of us are just barely hanging on.”
Building a Backbone
A reasonable step that imaging leaders can take today to help their facility embrace AI is preparing their IT infrastructure. IT departments face significant challenges when it comes to integrating AI into an existing workflow, Chang says, but that’s a necessary step if you want to actually see benefits once the technologies are ready to be implemented.
“AI is a critical tool, but you don’t build architecture for a tool—you build it for a solution,” Chang says.
A flexible, strong and standards-based platform is essential to enable the organization to capture, enhance, protect and share key data and digital analytics assets.
Instead of concentrating solely on the technology, Chang recommends departments focus on the end results they desire. Aim for improved efficiency, for instance, and 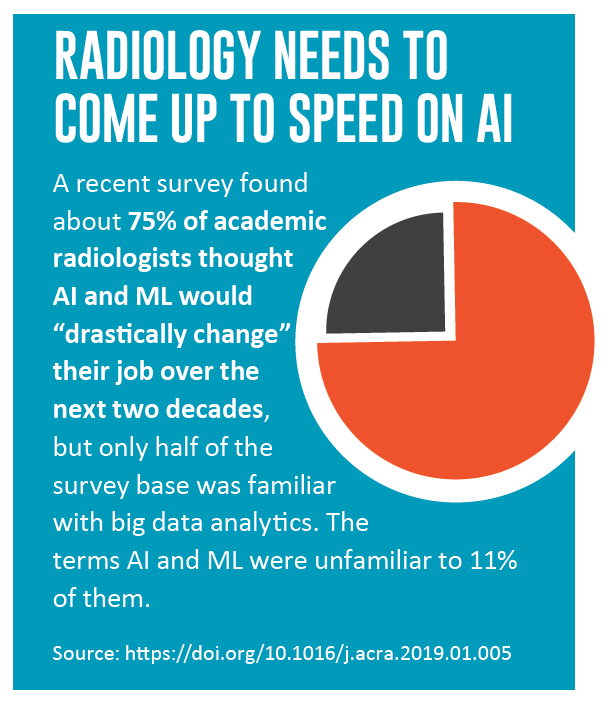 how AI can help make that a reality. C-suite executives care about improving efficiency because it can save time and, ultimately, money. To build a strategy to integrate AI into your standard workflow, speaking about it in those terms is the way to ensure you get the needed investments.
how AI can help make that a reality. C-suite executives care about improving efficiency because it can save time and, ultimately, money. To build a strategy to integrate AI into your standard workflow, speaking about it in those terms is the way to ensure you get the needed investments.
Radiologists need to be engaged in AI, he says, but realistic on expectations and timing. “The goal is not to be hyped about the technology’s capability,” he says. “You need to be hyped about an infrastructure and interested in improving efficiency and quality simultaneously.”
That’s where vast amounts of data and compute power converge, Wendt notes. “You need to make sure you have a good data processing or automated data pipeline,” he says. “You want to be able to plug in these platforms on the back end and have data automatically routed. [Data have] to be routed real time, processed real time, and make the full loop back to the radiologist real time before the radiologist even signs the report. And then loop back to the EMR.”
Making a Difference
One of the greatest ways AI can provide value to today’s radiologists is through improving day-to-day workflow and allowing them to be more efficient. Less time spent on more mundane tasks equals more time spent reading studies and helping patients. NLP can help with mundane tasks as automated image segmentation helps with labeling, measurement and comparing newer studies with prior studies.
Looking at AI with a broader brush stroke, the true difference machine intelligence will bring is in the care of individual patients and populations over time. Analyzing longitudinal data, improving insight and decision-making today and reaching back into that data as the evidence base evolves, best practices change and guidelines advance to offer more effective methods of diagnosis, prevention and treatment.
“I think as we move forward [over] the next five years, it’s not just going to be about the algorithms,” Bruce says. “It’s going to be about proving what is the real value to the people who ultimately are consuming it.”
Radiology, too, offers great value to the evolution of care aided by machine intelligence. Two researchers from the Japanese Radiological Society put it this way. “AI can be expected to gradually change clinical practice by helping radiologists practice with better performance, greater interrater reliability and improved workflow for more timely recommendations,” they wrote in the PLOS Medicine Special Issue on Machine Learning in Health and Biomedicine. “Radiologists will be important in labeling training datasets and developing new knowledge from image data. In the clinic, even if current deep learning approaches broadly excel in image interpretation, radiologists will continue to play central roles in the diagnosis of rare diseases and in the detection of incidental findings.”
For the doctor’s doctor, now is the time to consult AI and define the strategy to lead the charge to more consultative medicine.